By CrossRiverWatch Admin
Being a sponsored statement from the Cross River State Ministry of Health.
Monkeypox is a rare viral zoonosis (a virus transmitted to humans from animals) with symptoms in humans similar to those seen in the past in smallpox patients, although less severe. Smallpox was eradicated in 1980. However, monkeypox still occurs sporadically in some parts of Africa.
Monkeypox is a member of the Orthopoxvirus genus in the family Poxviridae.
The virus was first identified in the State Serum Institute in Copenhagen, Denmark, in 1958 during an investigation into a pox-like disease among monkeys.
Human monkeypox was first identified in humans in 1970 in the then Zaire Republic now the Democratic Republic of Congo in a 9 year old boy in a region where smallpox had been eliminated in 1968 and in 1996-97, another major outbreak occurred in the same country.
This was followed by reported cases of outbreaks in 2003 in the Midwest of the United States of America, marking the first reported occurrence of the disease outside of the African continent. Then in 2005, 2009 and between August and October 2016, another outbreak in the Central African Republic was contained with 26 cases and two deaths.
Infection of index cases results from direct contact with the blood, bodily fluids, or cutaneous or mucosal lesions of infected animals.
In Africa human infections have been documented through the handling of infected monkeys, Gambian giant rats and squirrels, with rodents being the major reservoir of the virus. Eating inadequately cooked meat of infected animals is a possible risk factor.
Secondary, or human-to-human, transmission can result from close contact with infected respiratory tract secretions, skin lesions of an infected person or objects recently contaminated by patient fluids or lesion materials.
The incubation period (interval from infection to onset of symptoms) of monkeypox is usually from 6 to 16 days but can range from 5 to 21 days.
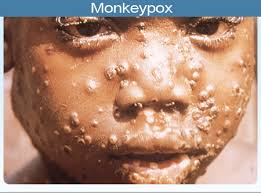
The first 0-5 days known as the invasion period is characterized by fever, intense headache, lymphadenopathy (swelling of the lymph node), back pain, myalgia (muscle ache) and an intense asthenia (lack of energy); and the skin eruption period which starts within 1-3 days after appearance of fever where the various stages of the rash appears, often beginning on the face and then spreading elsewhere on the body.
The face (in 95% of cases), and palms of the hands and soles of the feet (75%) are most affected.
The case fatality has varied widely between epidemics but has been less than 10% in documented events, mostly among young children. In general, younger age-groups appear to be more susceptible to monkeypox.
Monkeypox can only be diagnosed definitively in the laboratory where the virus can be identified by a number of different tests.
The differential diagnoses that must be considered include other rash illnesses, such as, smallpox, chickenpox, measles, bacterial skin infections, scabies, syphilis, and medication-associated allergies. Lymphadenopathy during the prodromal stage of illness can be a clinical feature to distinguish it from smallpox.
There are no specific treatments or vaccines available for monkeypox infection, but outbreaks can be controlled.
Vaccination against smallpox has been proven to be 85% effective in preventing monkeypox in the past but the vaccine is no longer available to the general public after it was discontinued following global smallpox eradication. Nevertheless, prior smallpox vaccination will likely result in a milder disease course.
In Africa, monkeypox infection has been found in many animal species: rope squirrels, tree squirrels, Gambian rats, striped mice, dormice and primates. Doubts persist on the natural history of the virus and further studies are needed to identify the exact reservoir of the monkeypox virus and how it is maintained in nature.
During human monkeypox outbreaks, close contact with other patients is the most significant risk factor for monkeypox virus infection.
In the absence of specific treatment or vaccine, the only way to reduce infection in people is by raising awareness of the risk factors and educating people about the measures they can take to reduce exposure to the virus.
Surveillance measures and rapid identification of new cases is critical for outbreak containment.
Health-care workers caring for patients with suspected or confirmed monkeypox virus infection, or handling specimens from them, should implement standard infection control precautions.
Restricting or banning the movement of small African mammals and monkeys may be effective in slowing the expansion of the virus outside Africa.